Subscribe to the newsletter "From Sputnik With News"
Most Read
April 19 Attack on Iran: Who is Responsible for It?
Yesterday
'History Will Remember': China Hits Out At US Opposition to Palestine's UN AdmissionYesterday
Watch Russian Military Robotic Vehicles Get Tested in Special Op Zone Yesterday
Russia Carries Out 34 Group Strikes on Ukrainian Military, Energy Facilities in Past WeekYesterday
US Media Claims Israel Targeted Air Defense Radar at Iranian Nuclear FacilityYesterday
Editor's Pick
Russian FM Lavrov’s Interview With Sputnik - Full Video
Yesterday
Blinken Protects Israeli Military Units Accused of Killings, Assault – ReportYesterday
Leaked NYT Style Guide Reveals Biased Reporting on Palestine-Israel ConflictYesterday
US Shows True Attitude to Palestinians by Casting Veto on State's Membership in UN - Russian Envoy18 April
US Benefits From Energy Price Hikes, Unlike Europe - IMF Chief18 April

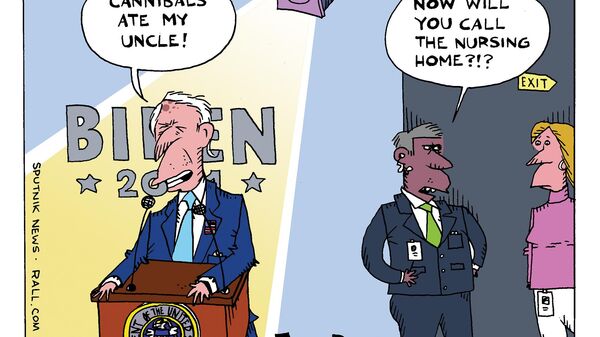
Tune In
Biden's Op-Ed on Ukraine and Israel; House Speaker Pushes $95 Billion for Forever War New FISA Bill Means More Surveillance and Less Privacy Speaker Johnson Defies Impeachment Threat to Unveil Nearly $100 Billion Funding Package Trump Trial Jury Selection, Assange Assurances, Boeing Whistleblower Testimony Kiev Jealous of Israel; Biden Rejects Calls to Free Assange; FBI Wanted Back Door to Telegram